Research from UHN’s Krembil Brain Institute has revealed potential disease-modifying effects of deep brain stimulation in Parkinson’s disease (PD), shedding new light on an old treatment.
PD is a neurodegenerative disease that affects millions of people worldwide. The disease is characterized by motor symptoms, such as tremors, stiffness, slowed movement, and impaired balance. These hallmark symptoms are caused by a progressive loss of neurons in an area of the brain that controls movement, called the basal ganglia.
For some people with PD, severe motor symptoms can be treated with a surgical procedure known as deep brain stimulation (DBS). This therapy involves implanting electrodes into specific brain areas where they deliver electrical impulses that correct abnormal neuron activity.
Despite the known benefits of DBS for relieving PD symptoms, there are still many unknowns surrounding how the therapy works and whether it can alter the course of the disease.
In a recent study published in Brain Stimulation, Krembil Brain Institute researchers Drs. Suneil and Lorraine Kalia provided evidence that DBS may serve as more than just a symptomatic treatment—it might actually alter underlying disease processes.
“A driving factor in most neurodegenerative diseases is the accumulation of misfolded proteins within or outside of brain cells,” explains Dr. Suneil Kalia, a Krembil Senior Scientist and co-lead of the study. “In PD, we see a buildup of a misfolded form of the protein alpha-synuclein (α-Syn), which disrupts neuron communication and eventually causes neuron death.”
According to Dr. Suneil Kalia, the search is on for treatments that can disrupt α-Syn production and aggregation, thereby slowing or even preventing PD progression.
To determine whether DBS has such disease-modifying effects, the Kalia labs examined whether high-frequency electrical stimulation, akin to that delivered by DBS electrodes, alters α-Syn.
“When we stimulated cultured brain cells, we saw significantly less expression and buildup of aggregated α-Syn. Within the brain, when we stimulated a small region of the basal ganglia called the substantia nigra pars compacta, we saw a lower overall level of α-Syn and less downstream effects,” says Dr. Lorraine Kalia, a Krembil Senior Scientist, Neurologist and co-lead of the study.
These findings hint at the potential of DBS to protect neurons and slow down the disease.
Interestingly, the team saw this benefit only when they simulated the substantia nigra pars compacta and not a nearby region that clinicians more commonly target in DBS.
Dr. Suneil Kalia is also a Neurosurgeon at Krembil Brain Institute and, together with his two colleagues, performs the largest number of DBS surgeries in Canada. “We regularly apply DBS to one of three functionally connected regions of the basal ganglia, depending on the patient and their specific symptoms—most commonly the subthalamic nucleus. DBS in this region can dramatically improve a patient’s motor symptoms, so we were somewhat surprised to see that it had no effect on α-Syn levels,” explains Dr. Suneil Kalia.
“This finding tells us that the disease-modifying actions of DBS may depend to some extent on the brain region being targeted—this will be an important consideration when optimizing treatment plans for individual patients,” he adds.
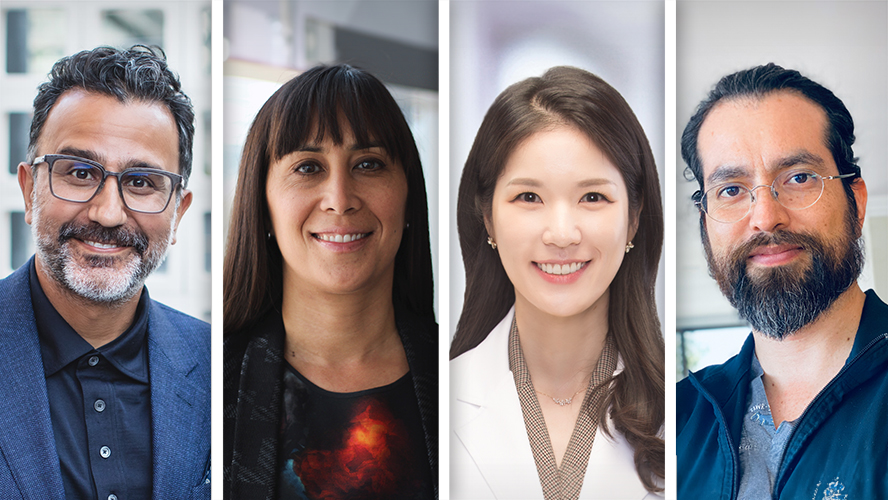
Dr. Eun Jung Lee and Dr. David Aguirre-Padilla are co-first authors of the study and former Postdoctoral Researchers in the Kalia labs. “DBS has been used to treat PD since the late 1990s but it is only now that we are learning about its disease-modifying properties. Our findings underscore the potential of harnessing existing therapies for neurological diseases in new ways,” explains Dr. Aguirre-Padilla.
Although more research is needed to determine exactly how DBS alters α-Syn, this study offers hope for millions of patients and their caregivers.
“The better we understand how DBS works, the more we can refine the therapy to enhance its benefits for each patient. This approach could really change the landscape of PD treatment,” concludes Dr. Lee.

PD affects more than 100,000 Canadians. DBS is a valuable treatment option for a subset of patients whose motor symptoms cannot be controlled by medication alone.
This work was supported by Parkinson Canada, Krembil Research Institute and UHN Foundation. Dr. Suneil Kalia is an Associate Professor of Surgery and holds the R. R. Tasker Chair in Stereotactic and Functional Neurosurgery at UHN. Dr. Lorraine Kalia is an Associate Professor of Medicine and holds the Wolfond-Krembil Chair in Parkinson’s Disease Research at UHN.
Lee EJ, Aguirre-Padilla DH, Fomenko A, Pawar G, Kapadia M, George J, Lozano AM, Hamani C, Kalia LV, Kalia SK. Reduction of alpha-synuclein oligomers in preclinical models of Parkinson’s disease by electrical stimulation in vitro and deep brain stimulation in vivo. Brain Stimul. 2024 Feb 10. Doi: 10.1016/j.brs.2024.02.005.

